The DNA Test Delusion
Answers to our greatest questions, we were told about a decade ago, could be ours if we just spat in a tube. Celebrities were using DNA tests to trace their ancestry on the hit TV show Finding Your Roots. A “Who’s Your Daddy” truck rumbled through the streets of New York City, offering paternity tests on the go. Angelina Jolie sent droves of women scrambling to get their DNA tested when she wrote a 2013 op-ed in the New York Times. Jolie, whose mother was diagnosed with breast and ovarian cancer and died at 56, credited a DNA screening with identifying a mutation in her BRCA1 gene that meant she had an elevated risk for cancer, too. In detailing her choice to get a double mastectomy, she helped cement the popular understanding that a single gene could mean the difference between life and death.
A few months after the op-ed ran, during an appearance on CBS This Morning, 23andMe Chief Executive Officer Anne Wojcicki said she was bringing the power of these sorts of DNA tests to everyone. Her startup would make testing affordable, she said, so it could build a massive repository of genetic data, one big enough to speed research and create a road map for living to age 100. Wojcicki cited her own DNA as proof of concept: She’d quit drinking after finding that she also carried a gene that heightened her risk of breast cancer. When co-host Gayle King said she’d heard some doctors were skeptical, Wojcicki brushed it off. “Anytime there’s a new technology for physicians, it’s a challenge,” she said. Then the conversation moved in a different direction, as co-host Norah O’Donnell asked whether 23andMe planned to usher in a future of designer babies.

Wojcicki shows off a purse printed with a DNA microarray at the Breakthrough Prize ceremony in April.Photographer: Tayfun Coskun/Anadolu/Getty Images
Around the time of that morning show appearance, Wojcicki’s team brought 1,000 of their DNA-testing spit kits to 23andMe’s first medical conference and managed to give away maybe five. Physicians breezed past her team to line up for Dippin’ Dots instead. In late 2013 the US Food and Drug Administration ordered 23andMe to stop selling its health tests until the company could prove they were safe and effective.
In a recent interview with Bloomberg Businessweek, Wojcicki looked back on that period with good humor. She says the early rejections only made her more determined. It was just a matter of time, she believed, until the medical community added genetic testing to its standard operating procedures. “When you start, you’re just naive about everything,” she says. “We thought, at some point, physicians would adopt it.”
Given more evidence, of course, the FDA later authorized the tests, and 23andMe became a household name. The problem, for Wojcicki and the rest of the DNA testing industry, is that all these years and millions of spit kits later, the doctors still don’t care. Mass-market genetic screenings remain well apart from the medical mainstream, and 23andMe has never made a profit . And unfortunately for Wojcicki and her peers, the reasons for that seem to be less about the stuffiness of the doctors than about the limits of genetic testing.
When researchers unveiled a working draft of the human genome in the early years of the 21st century, it was billed as a panacea. Within our DNA, the project’s boosters said, lay the keys to victory over almost everything that ails us. Drugs tailored to a person’s particular genetic code had the potential to cure diseases instead of merely treating them. Genetic risk assessments would drive people to eat and exercise in the ways they needed to avoid getting sick in the first place. Today, however, the biggest insight most people have gained from DNA testing is trivia about their ancestors’ countries of origin. Most doctors remain untrained in genetics, when to order a DNA test or what to do if a patient brings one in. Therapies targeting the human genome are few and far between, and they’re often too expensive for most people to afford.
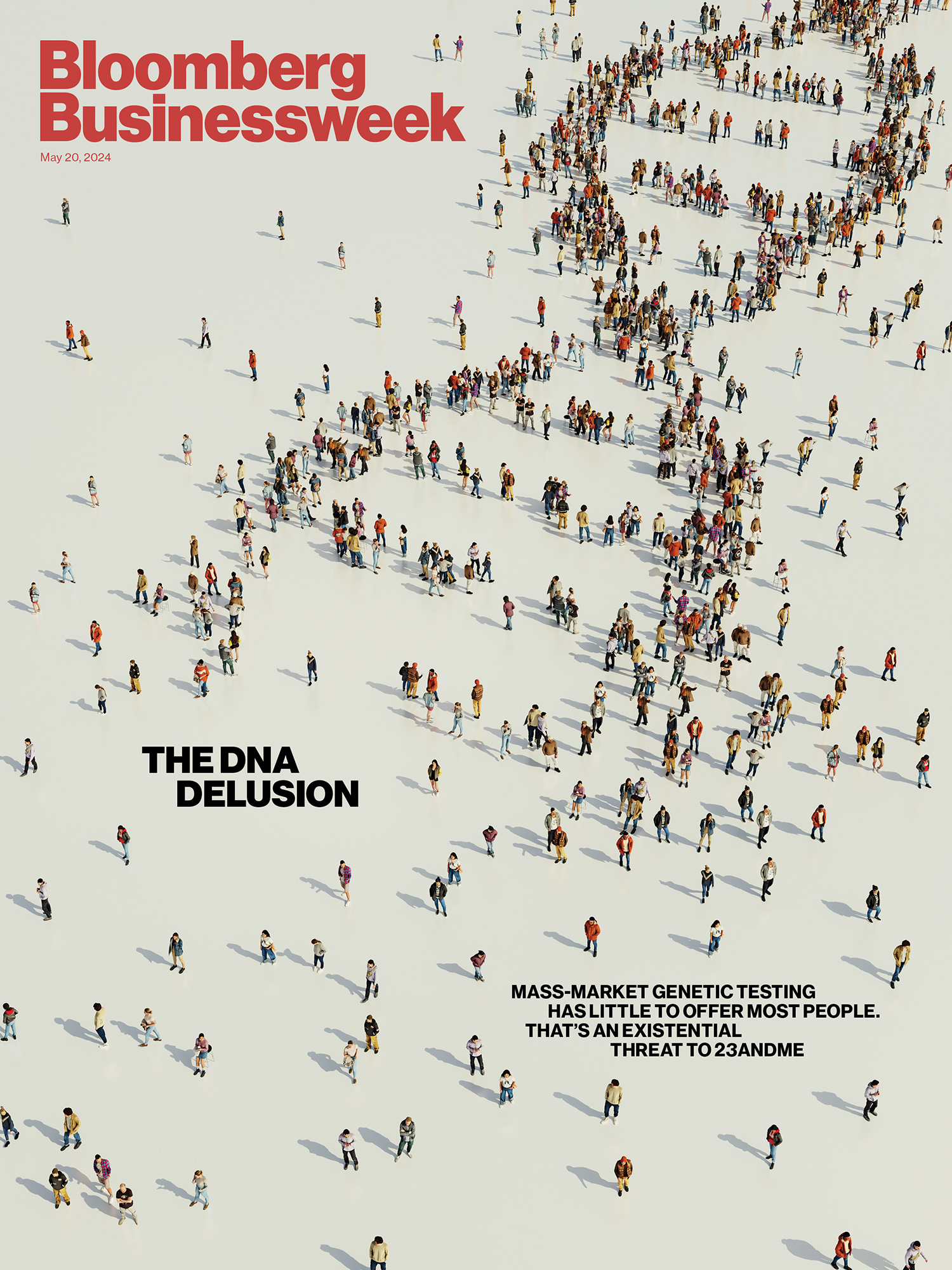


Featured in Bloomberg Businessweek, May 20, 2024. Subscribe now.Illustration: Saratta Chuengsatiansup for Bloomberg Businessweek
We’re still waiting, in other words, for health care’s great DNA revolution. And a growing contingent is starting to question whether genetic data simply isn’t of much use to the average person. “Everyone now is getting their genetic reports back and realizing that it’s not actually making a damn bit of difference when it comes to their health,” says James Tabery, a professor of philosophy and bioethics at the University of Utah and author of Tyranny of the Gene: Personalized Medicine and Its Threat to Public Health.
“I’m more confident than ever,” Wojcicki says. “But I think there’s also that reality that it’s not like gold dripping from trees.” Few have more riding on the next phase of applications from DNA testing than 23andMe. Over the past decade, it’s tried a lot of strategies to make personalized genetics profitable. It partnered with Big Pharma to develop drugs from DNA insights. It acquired a telehealth company. Most recently it rolled out a $999 yearlong testing subscription that includes full sequencing of the genome’s protein coding regions, two rounds of blood tests and analysis from a clinician. Still, it has yet to graduate from stocking stuffer to health care. As kit sales have slowed, investors have soured on the company’s longer-term bets, and its stock is on the verge of being delisted from the Nasdaq. (On May 10, the company said it had received an extension of 180 days to bring its share price back above $1, according to a filing with the US Securities and Exchange Commission.) 23andMe needs to find a way to increase sales, raise capital or slash spending, even as it struggles to close the gap between the practical uses of DNA testing and the hype.
Wojcicki acknowledges things aren’t going exactly according to plan. “We’re in an industry that is definitely figuring out what is that application of genetics in the clinical space,” she says. “It’s a little bit of a sector in crisis.”
Code has proven an imperfect genetic metaphor. DNA’s double helix structure, first revealed to the world in the 1950s, is made up of billions of base pairs of A’s, C’s, G’s and T’s. Each one of a person’s roughly 20,000 genes amounts to a stretch of those letters, and the ACGT makeup of individual genes can make the difference between brown eyes and blue ones, or attached earlobes and the free-swinging kind. In the 1980s and ’90s, a string of research breakthroughs began to pinpoint the location of individual genes for conditions such as Huntington’s disease and cystic fibrosis. The prospect of a full-length genetic code, then, seemed to promise that we could reverse-engineer the eradication of diseases by treating DNA as something akin to a programming language. If we could decrypt the code, we’d just have to figure out how to intervene in the disease genes—to switch the 1s to 0s, the ons to offs.
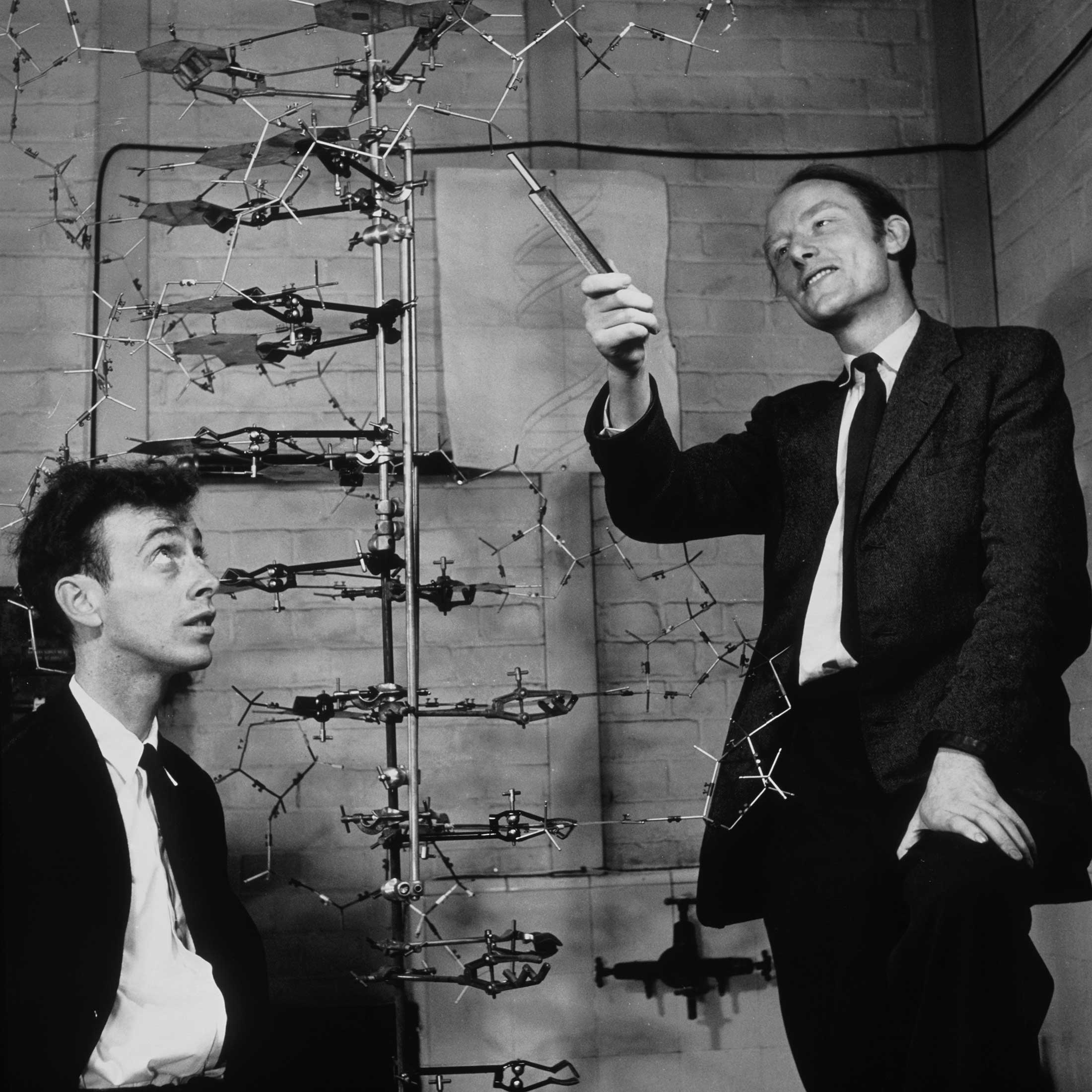


James Watson and Francis Crick, working with Rosalind Franklin and Maurice Wilkins, discovered the double helix structure in the 1950s.Photographer: A. Barrington Brown/Gonville & Caius College/Science Photo Library
As a team of international researchers drew close to finishing the Human Genome Project, the first full sequence of a person’s code, its backers made grand promises about the data’s potential. In 2000, President Bill Clinton said it would lead to cures for Alzheimer’s, Parkinson’s, diabetes and cancer. In 2003, at a celebration of the project’s completion at the National Museum of Natural History in Washington, Francis Collins, the scientist who led the endeavor, predicted that researchers would identify the genes responsible for those diseases within a decade, and that by 2020 “we will have a gene-based designer drug available for almost any disease that you can name.” Collins, who went on to run the National Institutes of Health, capped his remarks with a DNA-themed song to the tune of Del Shannon’s Runaway. He played guitar, and the audience clapped along to the chorus: “I wonder / wo-wo-wo-wo-wonder / Why / why why why why why / you’ve got an A / I’ve got a C there, what does that say? / Amazing DNA.”
Within a few years of Collins’ performance, new technology made it much easier to suss out teeny variations in DNA that can turn a healthy gene into a disease-causing one. Keeping up with the pace of discovery, the New England Journal of Medicine wrote in 2007, was like “drinking from a fire hose.” That same year, 23andMe shipped its first product, a $999 DNA test, with the help of $4 million in funding from Google. (At the time, Wojcicki was married to Google co-founder Sergey Brin.) Wojcicki and her co-founders said they planned to take the genetics revolution out of the lab and put it in people’s hands. “That any consumer with $1,000 can now capitalize on this project is a rare case of groundbreaking science overlapping with an eager marketplace,” Wired magazine wrote at the time.
We now know of about 10,000 diseases caused by mutations in single genes, but they are, for the most part, rare. Combined, they affect about 6% of the population, according to one estimate. Few are as genetically clear-cut as Huntington’s disease, which causes a debilitating and eventually fatal breakdown in the brain’s nerve cells. Everyone with the telltale mutation in their HTT gene, perhaps a handful out of every hundred thousand people, will develop the disease, leading to progressive decline in their mental faculties and motor skills. Small populations of people with monogenic diseases mean small markets for potentially lifesaving drugs. To date, most successful gene therapies have been prohibitively expensive, on the order of millions of dollars per patient.
Humankind’s leading killers, on the other hand, can rarely be defeated by flipping the switch on a single gene. The past decade of research has made clear that there isn’t usually one gene responsible for a person’s diabetes or heart disease. An unknown number of genes might play a role in the many bad things that can happen to your heart, and we understand very little about how those genes interact with one another. “The human genome was far more complex than anybody anticipated,” says Tabery, the bioethicist. What we do know is that while your genes might give you an increased risk of diabetes or heart disease, it’s not a foregone conclusion. Your environment, diet and exercise are factors of comparable or greater significance. And some of it is just random.
“Genetics is mainly usefully informative for conditions that are sufficiently uncommon that mass screening doesn’t make sense,” says Hank Greely, a law professor who directs Stanford University’s Center for Law and the Biosciences. “It’s just not compelling enough medically.”
Despite this shift in expert thinking, the popular narrative of DNA testing’s surpassing power endured for years. In 2017, Oprah Winfrey named 23andMe’s test kit one of her favorite things, calling it “the ultimate selfie.” In 2018, the National Institutes of Health, under the leadership of former Human Genome Project chief Collins, announced plans to sequence the DNA of 1 million Americans “to advance individualized prevention, treatment and care for people of all backgrounds.” In 2021, when it went public via a special purpose acquisition company founded by Richard Branson, 23andMe was valued at $3.5 billion.


A 23andMe saliva collection kit.Source: 23andMe
These days, though, the cliché isn’t that your test results will help you head off a fatal disease. It’s that they might break up your family. (Or, less often, help cops catch a serial killer.) As testing has slowed, 23andMe and its leading competitor, Ancestry.com, have collectively laid off hundreds of employees in several rounds of cutbacks. Branson has lost more than $150 million since 23andMe began trading, according to data compiled by Bloomberg.
The prevailing wisdom on how to make it to 100 is still the same old boring advice: exercise, eat well and get enough sleep. Even so, the idea that we all run on a code that can be decrypted and debugged—a code that explains who we are—is hard to give up. Wojcicki says her team isn’t going to.
“We need to combine genetics with family and personal health history, blood and RNA analysis and other factors to fully understand risks and best actions”
Genetic data may not be the cure-all we once dreamed of, but it still has the potential to deliver a holistic health assessment, according to Wojcicki. Some of the latest tools the company is using to do that are called polygenic risk scores, statistical models that calculate a person’s risk of disease by analyzing many genetic variants. The value of genomic screening is twofold, she says: It gives guidance for preventive care and a road map for personalized drug treatments. “Everyone gets something,” she says. “Every single person.” Of course, if you look at enough risk factors, eventually everyone will be at risk for something.
Wojcicki had just returned from a ski trip to Montana with her kids and Noura Abul-Husn, the company’s vice president for genomic health, when she sat down for a February interview at 23andMe’s offices in Sunnyvale, California. A storm had littered the roads around the headquarters with downed trees, which seemed very on-the-nose for the moment. A Wall Street Journal headline had just called 23andMe “virtually worthless.” The company was fighting a class-action lawsuit related to the theft of customer data by hackers. Its stock was trading at about 66¢ a share. Wojcicki, still dressed in her plane clothes after rushing from the airport to drop her kids off at school, could have been forgiven some grumpiness. Instead, she was decidedly upbeat. Her main complaint was that the bad weather didn’t wind up gifting her family an extra ski day.
“Relentless” isn’t a strong enough word for Wojcicki’s brand of optimism. The CEO attributes her sunny outlook to a solid team and a 10 p.m. bedtime. If having its main product outlawed for several years didn’t kill the company, she says, the latest decline is just another hiccup. She does acknowledge that the pressures of being a public company have made things tenser and quieter. “We were so lucky in 2013 that we weren’t public,” she says. “It’s a whole new level of complexity, because you are very much restricted about what you can say.”
Unbowed by disinterest from doctors, Wojcicki hired her own by buying telehealth startup Lemonaid Health for $400 million in late 2021. Last fall, in the face of slackening demand for its cheaper testing options, 23andMe introduced Total Health, its $999 tests-and-coaching subscription. (Each extra year costs $499.) Rather than try to win over insurers, “we’re really trying to create a different system that’s self-pay,” she says. 23andMe has so far not seen the subscription rates it expected, Wojcicki says, so it needs to give the people who have bought in more opportunities to buy things. Blood tests. Doctor visits. Pharmaceuticals. Care plans. An app store for DNA. “We can have an all-in service for individuals who are looking to really know about themselves, like, what the risk factors are and what can they do?”
Abul-Husn says Total Health, 23andMe’s latest bet, is focused on care plans for people with more than 100 genes linked to 55 conditions that are broadly considered “actionable,” including forms of cancer, cardiovascular disease, metabolic disease and neurological disorders. Total Health might recommend that a person it has identified as at risk for heart disease, for example, consider taking statins to lower their cholesterol sooner than a doctor might otherwise suggest. 23andMe’s most valuable asset may be its database of 15 million customers, which it continues to mine for drugs. The company has used its customer data to identify dozens of potential treatments for development. It is conducting clinical trials for two of those and has a stake in a third trial conducted by GSK Plc.
Ancestry and other rivals, however, have mostly struck out in the areas 23andMe is pursuing. Helix Inc. shut down a gimmicky app store. Color Health Inc. killed its consumer-facing testing. Both have shifted focus: Helix to partnerships that incorporate genetic testing into research and primary care for large numbers of participants, Color to cancer screenings, including DNA testing, as part of employer benefit packages. Ancestry shuttered its own DNA-based health analysis product inside of two years. “To connect all those dots from risk to diagnosis to action is the hard part,” says former Ancestry CEO Margo Georgiadis, who now runs Montai Therapeutics. “We need to combine genetics with family and personal health history, blood and RNA analysis and other factors to fully understand risks and best actions.”
And drug development takes many years and lots of money, with few guarantees the return will cover the investment. So far, there have been only a few instances where genetics has directly led to a brand-new drug. The biggest blockbusters of our time—Ozempic and its sibling GLP-1s—came from an investigation into how the GLP-1 hormone works.
To see what Total Health could discern, on behalf of Businessweek, I took a full battery of its tests, starting with the familiar spitting into a large plastic tube. Most consumer DNA testing relies on genotyping. Total Health includes sequencing the entire exome, the portion of DNA widely believed to be responsible for the vast majority of disease-causing genetic variants. Sequencing delivers a far more complete picture of the genome. 23andMe’s standard tests can identify whether someone has certain harmful variants of BRCA genes that are commonly associated with breast cancer, but it can’t rule out whether a person has other problematic variants of the BRCA genes. Sequencing can decode any variant of a BRCA gene, not just identify preselected ones. By combining this with blood testing and a clinician consult, the company hopes to give people a well-rounded picture of their health.
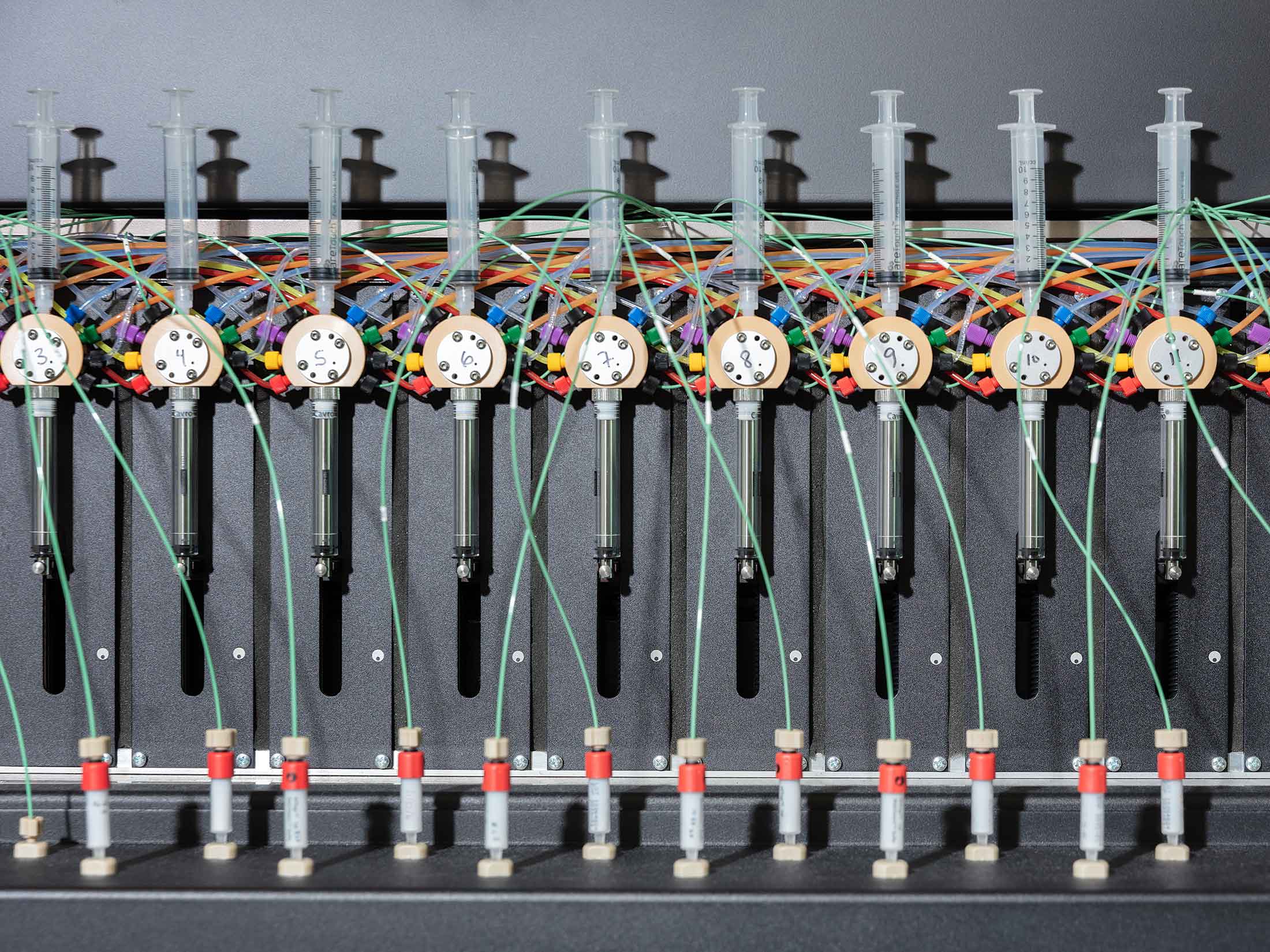
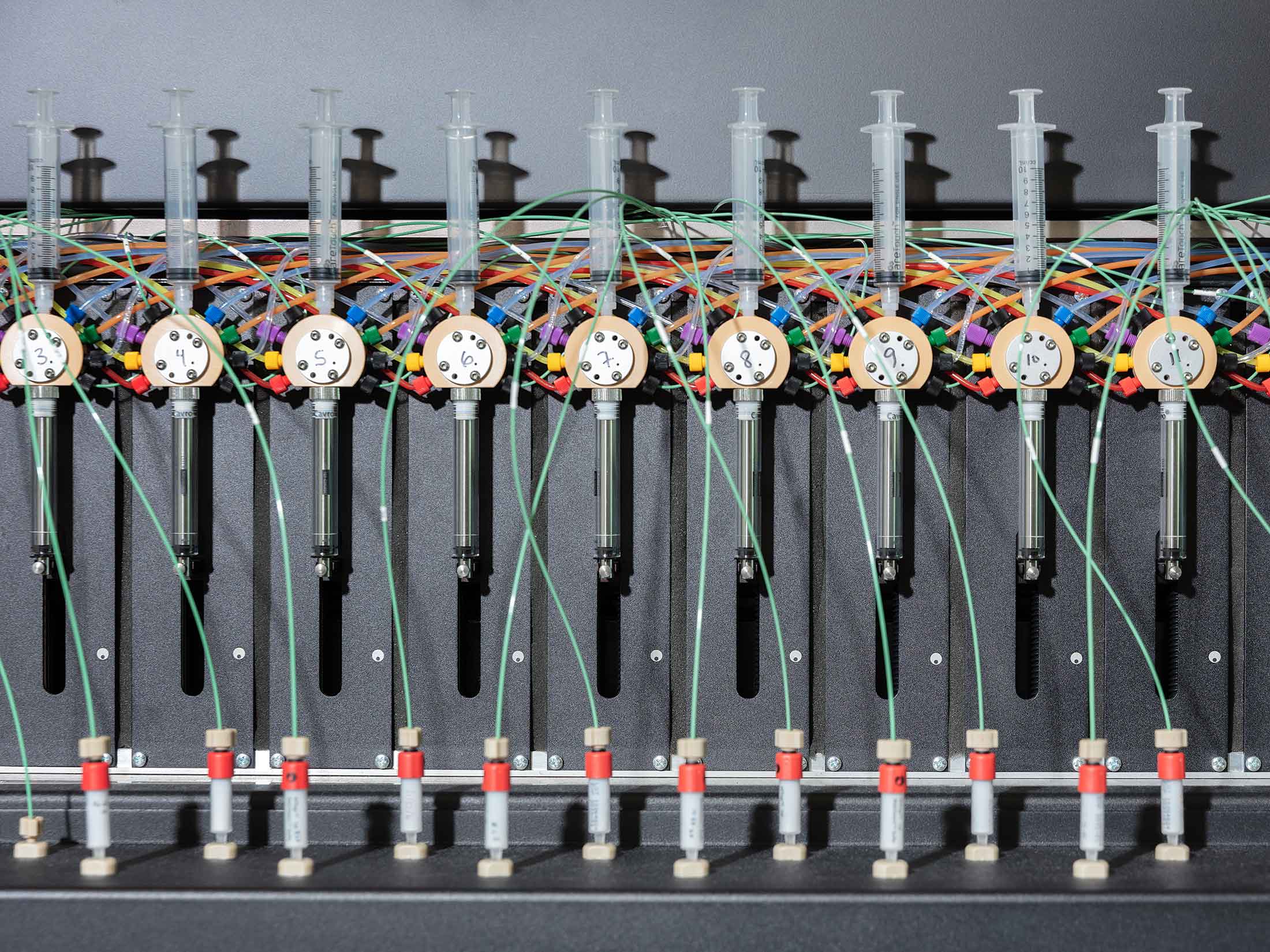


A 23andMe “Protein Maker,” designed to isolate and purify samples of DNA, proteins and antibodies.Photographer: McNair Evans
After months of waiting, 23andMe said my results were ready in early May. I logged into my account and clicked the link for my “Health Action Plan.” Its conclusions were anticlimactic: “Keep doing what you’re doing. We don’t have any activities to recommend for you at this time.”
After spending 20 minutes filling out a detailed family history, I talked to a physician. “Sometimes the family history can tell us more than the genetics, believe it or not,” she said. After having the same sort of lengthy chat about my diet and other habits that I might have at my annual physical, she walked me through my results. I had a slightly elevated risk of celiac disease and a more moderate risk of eventually developing glaucoma. She said to not worry about the celiac—I would know by now if I had a gluten intolerance, and my consumption of avocado toast suggested I did not. As for the glaucoma, she said, the only real thing I could do was generally strive to live a healthy life, which I was already doing. She didn’t have any real recommendations. In her after-visit summary she wrote: “Keep up the great work.”
Not having a harmful variant on one of the 33 genes associated with cancer that 23andMe sequenced doesn’t mean I won’t one day get it. As the report explained, “only 5-10% of cancers are believed to be hereditary.”
What I’m more certain about is that if I can cut down on stress-eating Girl Scout Cookies while on deadline, fit in daily workouts before work and finally drop the 20 pounds I’ve gained over the past decade, it will make a significant difference to my health. I don’t need a DNA test to tell me that. And for the average person, the advice to eat healthier, move more and sleep better is about as much insight as a DNA test can offer.
In response to the sharing of my results, Abul-Husn says broadly that a DNA test will have value to “virtually every person” when you include polygenic risk scores and pharmacogenetics, which analyze how genetics might affect a person’s response to drugs. More than 90% of subscribers to one of the company’s premium subscriptions, 23andMe+, have an actionable result, she says.
The difference may lie in what you consider actionable. Greely, the Stanford professor, had a different takeaway. “You are, I think, going to prove to be representative of about 90%-plus of the population,” he said. I have a boring genome. Most people do.
“Everyone’s like, ‘No one’s going to change behavior.’ ” That’s kind of like, ‘I’ve given up on you already before it’s even started’ ”
The most powerful revelations of the genome can sometimes be not who we are, but who we aren’t. In my own family, DNA testing got one relative’s heritage dead wrong but correctly revealed that a second was not, in fact, genetically related to their father. (Long story.) It’s a common occurrence these days. A 2022 YouGov survey found that about a third of test takers learned about close relatives they previously didn’t know about. Consumer DNA testing has broken and remade so many families, it hardly grabs headlines anymore.
For some people, DNA winds up being an especially important piece of life’s puzzle. For most, it’s starting to look like it’s just another data point. “We live in a society where almost no one exercises enough, no one eats enough fruits and vegetables,” says Timothy Caulfield, a professor of health and science policy at the University of Alberta. “It seems almost absurd that we’re focusing on these slight genetic differences between individuals and suggesting that’s going to make a significant change.”
To date, peer-reviewed studies have often found that people don’t really make large-scale behavioral changes based on DNA tests. The people most likely to benefit from something like Total Health, Caulfield says, were probably already proactive about their health care to begin with. “They’re the worried-well, the wealthy that are already highly, perhaps overly, engaged in their health,” he says. “We’re not looking at this profound revolutionary shift.”
23andMe says a customer survey showed 76% of respondents reported a positive behavior change after viewing their 23andMe results, and it says the evidence of positive health effects is mounting. Wojcicki dismisses the naysaying as a lack of patience for patients. “Everyone’s like, ‘No one’s going to change behavior,’ ” she says. “That’s kind of like, ‘I’ve given up on you already, before it’s even started.’ ”
Decoding the human genome, of course, has led to incredible breakthroughs. It has given us a better understanding of how some diseases work, and even helped to come up with non-genetic therapies for them. It has helped us to diagnose rare diseases. Carrier screening and genetic testing ahead of IVF implantation have helped countless parents avoid passing on genetic conditions, while newborn screening helps to identify conditions such as cystic fibrosis early, before symptoms appear. Some evidence suggests it might be worth screening large swaths of the population for genes linked to hereditary breast and ovarian cancer, a form of colorectal cancer called Lynch syndrome and a condition called familial hypercholesterolemia. Those genes are rare but not that rare, and regular screenings seem to make a big difference. Those are the genes Helix screens for on behalf of its health-care partners, the genes insurers are most willing to pay to spot. Even then, though, it’s unclear whether people themselves want that information. When the 2018 NIH research program began returning test results to its 100,000 participants, only about half wanted them. And those results were free.
Wojcicki isn’t the only one who still thinks DNA can play an outsize role in an individual’s health. About 2.4% of the NIH program’s participants came back with an actionable variant of concern. Collins, the former NIH chief, acknowledges that the landscape of genetic testing has been far more complex than anticipated, but says he’s still bullish the genome will eventually deliver on its full promise. In the meantime, he says, being able to tell 2.4% of people they are at risk of developing disease is extremely valuable. “I get a little defensive about this,” says Collins. “People say, ‘Well, you know, the Human Genome Project said all this was going to happen, and here we are and I don’t see it.’ Well, look, people, it’s there. It may not be quite the places we expected, but it’s happening.”
Other businesses are placing their bets. Robert Green, a Harvard geneticist, recently went public with Nurture Genomics, a company that promises to “provide ongoing personalized support to deliver genomic-guided care early in life” after screening the DNA of your newborn. “If you combine genetic risk with targeted care and surveillance for those individuals at higher genetic risk, I believe that you can change outcomes,” Green says. Just as it was impossible, decades ago, to predict what we might learn from decoding the genome, we can’t yet be sure what else we might find as we continue to untangle its myriad connections.
Greely, who 20 years ago believed DNA testing would revolutionize health care, says it’s possible that in another decade or two a standard checkup will include genetic screening, but he doubts it’ll do much good. “Every utopian says, ‘Oh, we’re almost there. We just have to try a little harder,’ ” he says.
In the end, that is pretty much what Wojcicki is saying. She still envisions 23andMe becoming a “true preventative care service” that remains apart from the health-care system but connected to it. If she has any hope of making that happen, she’ll have to avoid running out of cash. In February, she told Businessweek she might split 23andMe’s drug development business from its consumer business. More recently, she told board members she is proposing to acquire the company in a potential go-private transaction. In a filing, Wojcicki indicated she plans to maintain control of the company and “will not be willing to support any alternative transaction.”
In her interviews with Businessweek, she’s held firm to her grander vision. “Our ambition is not just an elite few million people,” she says. “Our ambition is we become a cornerstone.” And how, exactly, does she plan to do that? “Perseverance,” she says. “One day we’ll look back—I don’t know what day, what year it will be—and we’ll be like, ‘They’re an overnight success.’ ” —With Ben Stupples
Read next: A Massive Therapy Hack Shows Just How Unsafe Patients’ Files Can Be
(Updates to include results of a YouGov survey in the 32nd paragraph. An earlier version of this story corrected a reference to an NPR story on preschool admissions in the first paragraph.)
Jonathan Latham, PhD
